Introduction
Lower back pain in pregnant women is common and 30% of them require bed rest as a result [1]. Meanwhile, sciatica associated intractable pain occurs in approximately 1:10,000 pregnant women [1]. The occurrence of lower back pain and its severity are affected by hormone changes, weight gain, shift in center of gravity leading to disc bulging or herniation and relaxin levels, which contribute to the sliding mobility of the sacroiliac joints, widening of the pubic symphysis, and laxity of the posterior longitudinal ligament [2].
Conservative therapy, such as stretching, acupuncture, and core training, should be tried as first line interventions and analgesics, such as nonsteroidal anti-inflammatory drugs, may be recommended following the risk classi’¼ücation guidelines for drug use in pregnancy. In non-pregnant patients, disc length is a predictor for surgical treatment or nerve block success [3]. However, there are no definitive guidelines for nerve block and drug combinations in pregnant women with sciatica or lower back pain.
This case report aimed to investigate the efficacy of epidural catheter insertion and intermittent local analgesic administration in a pregnant woman, presenting with severe, acute lower back pain and sciatica.
Case Report
A 30 weeks 32 old age prim gravida woman whose weight and height were 62 kg and 162 cm, visited the emergency room with a three day history of lower back pain and right leg pain. One day ago, she felt pain abruptly on back and right leg radiating pain with visual analogue scale 3. But the pain aggravated with movement and increased visual analogue scale (VAS) (Where VAS 0 = no pain, 10 = severe pain) 8. The leg pain was located in the right gluteal region of the leg and associated with numbness. At emergency room, pain severity was assessed as 9-10 using VAS. On physical examination, straight leg raising test (SLRT) revealed 15/90. However, knee and ankle jerk tests were normal. Motor function did not reduce on the flexion or extension of knee, ankle and toe.
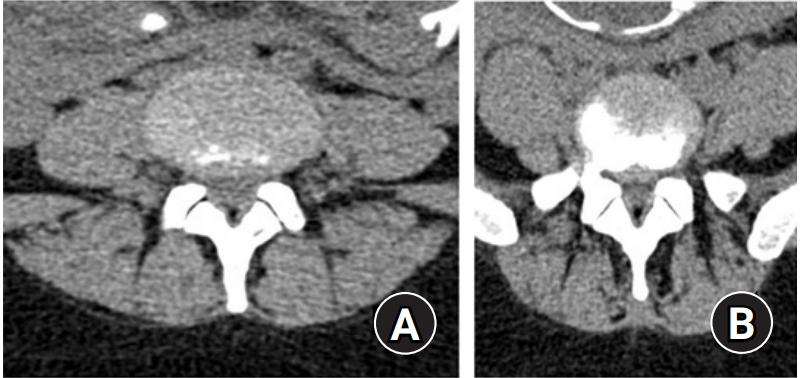
Despite intravenous administering pethidine 25 mg 4 times per day for pain relief, the patient was unable to maintain a supine position. The patient requested surgery to alleviate pain to neurosurgeon. Therefore, image workup should be needed for severity of disc herniation or stenosis. But magnetic resonance images (MRI) could not be obtained because the patient did not bear supine position over several minutes. As a result, diagnosis was based on lumbar radiography and computed tomography (CT) scans after obstetric consultation for fetus safety, which confirmed lumbar 4/5 and 5/S1 disc bulges (Fig. 1). The patient requested surgery to alleviate pain after diagnosis but the surgeon recommend to neuroaxial block for symptom relief before the operation to minimize the risk of early delivery. Caudal block with ultrasound was conducted by neurosurgeon and the doctor injected the drugs which consisted 1% lidocaine 0.5 mL, dexamethasone 2.5 mg with normal saline 4 mL. But patient complained severe pain during injection, total 2.5 mL of drugs was injected. The symptoms did not relieved, therefore neurosurgeon consulted pain clinic to decrease pain.
We decided to insert an epidural catheter for drug administration several times because single injection of local anesthetics combined with steroid or not, might result short-term effects. During the procedure, the patient could bear standing and leaned position, so the intervention was conducted standing position (Fig. 2A). The catheter position was checked with fluoroscopy to minimize the risk of intravenous injection of local anesthetics in the epidural space which could result in the drugs being passed to the fetus. Real-time fluoroscopy revealed intravenous injection of contrast material (Bonorex 300 Inj┬«, Iohexol 647 mg/mL) at the first attempt of epidural catheter insertion at L5/S1. In the second trial, we inserted the catheter at L4/5 and confirmed the epidural space without vessel contrasted (Fig. 2B). Total amount of contrast material we administrated through epidural catheter, was 5 mL. The catheter tip located was located at L3/4 and 6 mL of 0.15% ropivacaine was administered. We used contrast material 5 ŌĆō 6 mL for confirmation correct epidural catheter location.
The patientŌĆÖs pain was reduced to VAS 4-5 after several minutes, allowing her to lie on the bed and fall asleep. The fetal heart rate was checked with an ultrasound device and did not reveal arrhythmia. After the first day, two more 6 mL injections of 0.15% ropivacaine, once per day, were administered and reduced pain to a final VAS score of 2 - 3. The patient was discharged five days later and observed for complications. Two weeks after discharge, the patient visited our clinic and stated she had paresthesia with a VAS score of 2 - 3. About two months later from discharge, the patient gave spontaneous vaginal delivery.
Discussion
In a systemic review, MRI was recommended as the safest method for diagnosis of disc herniation and lower back pain during pregnancy [4]. Because of high radiation exposure, CT should not be recommended as the first diagnostic tool; however, after 25 weeksŌĆÖ gestation, there is no teratogenic effects from CT at doses less than 100 mGy. Usually, the effective radiation dose range of lumbar or thoracic spine CT scan is less than 10 mSv [5]. The effective radiation dose of the lumbar spine series with oblique view is 1.91 mSv and the total radiation dose for this patient after her ER visit was estimated to be less than 20 mSv. We checked fluoroscopy approximately ten times in the pain clinic to confirm the proper location of the epidural catheter. The interlaminar epidural block took 46.6 ┬▒ 4.2 sec by mean to administer and radiation exposure was approximately 5 mSv per administration [6]. Therefore, her total radiation exposure was less than 25 mSv, far below the teratogenic dose.
Iohexol which is used for contrast material in flouroscopy is categorized Food and Drug Administration (FDA) class B agent. In human, it is not observed adverse effect. But informed content should be obtained before administration of all drugs in pregnancy. In some study, nonionic contrast was detected in gastrointestinal tract of neonate in other study [7]. But nonionic contrast transferred though placenta, did not affect neonatoal thyroid-stimulating hormone (TSH) [8]. We used contrast material for confirmation epidural catheter location in epidural space but, we thought little affect to fetus because contrast material was small amount.
In this case, we could control pain through an epidural catheterization without any side effects in the mother or fetus. Up to 10 % of epidural catheters puncture and advanced into the blood vessels of epidural space because of increasing abdominal pressure such as mass or pregnancy [9]. Most of that cases was detected but 1% of all epidural catheters inserted may not be identified whether catheter is lying intravascular. Serious complications occurs local anesthetics injection through catheter lying in epidural vessels. Vascular networks of epidural space increase and vessels are engorged in the third trimester of pregnancy [10]. Ultrasound guided intervention is useful and safe tool without radiation exposure, especially to pregnancy. However Ultrasound guided spine injection reveals possible limitation such as the inability to accurately detect intravascular injection in such deep injections especially epidural space which is partially covered by bones [11]. Local anesthetic toxicity via accidental intravascular injection causes dizziness, disorientation, drowsiness, convulsions, unconsciousness, coma, and respiratory depression and arrest. ThatŌĆÖs why we concerned fluoroscopy guided intervention in this patient to detect intravascular placement of epidural catheter.
In some case report, surgery following epidural block, was conducted for pregnant woman. Two separate injection of epidural block did not prevent motor weakness caused large sequestrated disc fragment [12]. In the other case report, relatively high dose steroid injection (triamcinolone 80 mg mixed with 6 mL normal saline) was done by ultrasound guided caudal block [13]. In our case, we thought several times injection of drugs to epidural space should be needed because caudal block failed to relieve pain. Repetitive administration of ropivacaine through epidural catheter in a rat model of neuropathic pain, revealed a definite analgesic effect [14]. ThatŌĆÖs why we conducted epidural catheter insertion for injection of local anesthetics. In this case, we used ropivacaine through an epidural catheter and found that pain decreased in the pregnant patient. However, ropivacaine can transfer to the fetus through the placenta. A study on the delivery of local anesthetics in epidural analgesia, where 15 mL of 0.1% ropivacaine (15 mg) followed by 10 mL.h-1 was administered to the mother, showed that ropivacaine was transferred to the fetus, with a concentration of 0.09 (0.08) mg.L-1 detected in umbilical blood; however, this did not affect neurobehavioral function [15]. This indicates that intermittent ropivacaine injection via an epidural catheter may be safe for the mother and fetus. The fetal vein/maternal artery concentration ratios (F/M ratios) of lidocaine and ropivacaine in dual-perfused human cotyledon model showed higher in lidocaine than in ropivacaine [16]. 0.5% epidural lidocaine plus fentanyl during labor revealed motor block significantly high than ropivacaine 0.08% plus fentanyl [17]. Therefore, administration of ropivacaine through epidural catheter to reduce pain in this patient had some benefits for mother and fetus.
To conclude, epidural catheter insertion and intermittent local anesthetic injection were effective methods for the treatment of lower back and sciatica in our patient without side effects and this suggests that this treatment may be effective for similar patients.